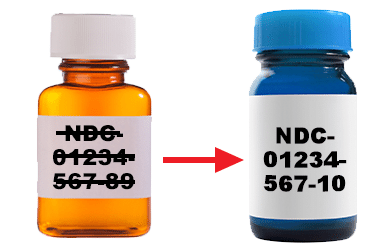
Genentech Access Solutions – Medicare Beneficiary Identifier (MBI) Update
- Katrina Williams
- October 17, 2019
- Administrative
- No Comments
Genentech Access Solutions – Medicare Beneficiary Identifier (MBI) Update This PDF provides important information about The Centers for Medicare & Medicaid (CMS) transition from the use of the Health Insurance Claim Number (HICN) to a Medicare Beneficiary Identifier (MBI) number, and how Genentech Access Solutions is addressing this conversion. Beginning January 1, 2020, Genentech Access…